
Case Studies
This section presents case studies where colleagues in Greater Manchester (and beyond) share their experiences and learning of how they tackled digital health inequities in their projects.
Developing Accessible Digital Health Software
 As a digital health software team, our aim is to build software to support health research across multiple disease areas and conditions. A key focus for us is co-designing websites and mobile apps with our target population to ensure the digital platforms that we build will be usable, useful and engaging. To do this, we work intensively with our end users to understand their accessibility needs and to create software that responds to their requirements.
As a digital health software team, our aim is to build software to support health research across multiple disease areas and conditions. A key focus for us is co-designing websites and mobile apps with our target population to ensure the digital platforms that we build will be usable, useful and engaging. To do this, we work intensively with our end users to understand their accessibility needs and to create software that responds to their requirements.
We currently work across a digital health portfolio of 20+ research projects, many of which are funded by the National Institute of Health Research (NIHR) or the Medical Research Council (MRC) in the UK. Most of these projects are focused on building software to support under-served populations.
Across our projects, ‘under-served populations’ are defined in different ways but within our current portfolio ‘under-served’ includes: people living with serious mental illness, people from economically-deprived areas and people living with multiple chronic conditions.
Improving the equity of digital health technology by using the Health Equity Impact Assessment Digital Health supplement (HEIA-DH)
 The rapid advance of digital health creates an imperative to focus attention on health equity. A team of researchers at the University of Toronto and the Centre for Addiction and Mental Health (CAMH) in Toronto, Canada, proposed the Digital Health Equity Framework (DHEF) to prompt service providers, organisations and tech developers to consider health equity when designing and implementing digital health technologies. The DHEF highlights social, cultural and environmental factors that shape how we interact with digital healthcare, creating “digital determinants of health,” including: access to digital health resources; use of digital resources for health seeking/avoidance; digital health literacy; beliefs and values about digital health; and integration of digital health resources into community and health infrastructure.
The rapid advance of digital health creates an imperative to focus attention on health equity. A team of researchers at the University of Toronto and the Centre for Addiction and Mental Health (CAMH) in Toronto, Canada, proposed the Digital Health Equity Framework (DHEF) to prompt service providers, organisations and tech developers to consider health equity when designing and implementing digital health technologies. The DHEF highlights social, cultural and environmental factors that shape how we interact with digital healthcare, creating “digital determinants of health,” including: access to digital health resources; use of digital resources for health seeking/avoidance; digital health literacy; beliefs and values about digital health; and integration of digital health resources into community and health infrastructure.
The Manchester Digital Pain Manikin
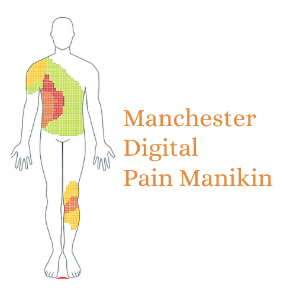 Pain is more common among ethnic minority groups in Greater Manchester than among white British. Differences in pain treatment and outcomes may partly be explained by differences in people’s pain beliefs and reporting behaviour (i.e., when, how and to whom people report their pain). This is why, as part of research programme called the Manchester Digital Pain Manikin, we explored the acceptability and feasibility of daily pain self-reporting using a smartphone app in people with chronic pain across different ethnic backgrounds. Click here to find out more.
Pain is more common among ethnic minority groups in Greater Manchester than among white British. Differences in pain treatment and outcomes may partly be explained by differences in people’s pain beliefs and reporting behaviour (i.e., when, how and to whom people report their pain). This is why, as part of research programme called the Manchester Digital Pain Manikin, we explored the acceptability and feasibility of daily pain self-reporting using a smartphone app in people with chronic pain across different ethnic backgrounds. Click here to find out more.
OPTimising engagement in routine collection of Electronic Patient-Reported Outcomes (OPT-ePRO)
 Routinely collecting patient-reported outcomes (PRO), such as symptom or quality of life questionnaires, can improve care and outcomes for people with chronic kidney disease and other long-term conditions.
Routinely collecting patient-reported outcomes (PRO), such as symptom or quality of life questionnaires, can improve care and outcomes for people with chronic kidney disease and other long-term conditions.
Collecting PRO data digitally (by asking people to use their smartphone or tablet), ensures that PRO data collection is feasible and sustainable as part of usual care pathways. However, previous research by the OPT-ePRO team suggested that people with kidney disease who are older or from socially deprived areas, are less likely to engage with electronic PROs (ePROs) and may therefore be vulnerable to digital health inequities. They may feel they lack digital skills, have no access to a digital device or the internet, have concerns about data privacy, or do not see the benefit for their health.
The REmote MOnitoring of Rheumatoid Arthritis (REMORA) research programme
 REmote MOnitoring of Rheumatoid Arthritis (REMORA) is a research programme to develop, evaluate and scale up an integrated symptom tracking intervention. This intervention enables people with RA to track their symptoms daily using an app on their smartphone (see image) and share and discuss the results with their clinical team. The tracked symptom data is available in (1) the REMORA app for patients to better self-manage their condition, (2) the hospital’s electronic health record system for clinical teams to make better and shared treatment decisions, and (3) a central repository for researchers to answer patient-important questions. Click here to find out more.
REmote MOnitoring of Rheumatoid Arthritis (REMORA) is a research programme to develop, evaluate and scale up an integrated symptom tracking intervention. This intervention enables people with RA to track their symptoms daily using an app on their smartphone (see image) and share and discuss the results with their clinical team. The tracked symptom data is available in (1) the REMORA app for patients to better self-manage their condition, (2) the hospital’s electronic health record system for clinical teams to make better and shared treatment decisions, and (3) a central repository for researchers to answer patient-important questions. Click here to find out more.
What factors have impacted on older people’s (75+) access/experience of public services during COVID-19?
 We know the digital divide and health inequalities often intersect, with groups such as older adults tending to be the most likely to have a need to access healthcare whilst being the group most likely to experience digital exclusion. Although use of the internet is increasing across all age groups, nearly half of people aged 75 and over have not used the internet within the last three months and over a third have never used it. The COVID-19 pandemic does not seem to have led to substantially higher numbers of older people getting online. Older adults who are at further risk of digital exclusion include those on low incomes, those living in social housing, living with disabilities, living in rural areas and those for whom English is not their first language.
We know the digital divide and health inequalities often intersect, with groups such as older adults tending to be the most likely to have a need to access healthcare whilst being the group most likely to experience digital exclusion. Although use of the internet is increasing across all age groups, nearly half of people aged 75 and over have not used the internet within the last three months and over a third have never used it. The COVID-19 pandemic does not seem to have led to substantially higher numbers of older people getting online. Older adults who are at further risk of digital exclusion include those on low incomes, those living in social housing, living with disabilities, living in rural areas and those for whom English is not their first language.
In this project we aimed to gather insight around factors that may contribute to older adults’ (75+) digital participation in Greater Manchester (GM). This directly aligned to the ambitions of the GM Digital Inclusion Task Force. Click here to find out more.
